Understanding TMJ and TMD
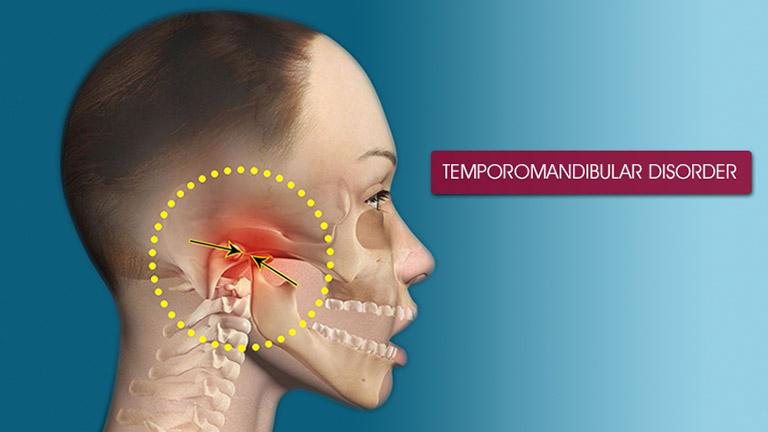
The temporomandibular joint (TMJ) is a critical hinge connecting the lower jaw (mandible) to the skull’s temporal bone, enabling essential movements like chewing, talking, and yawning. This joint is unique in its ability to slide and rotate simultaneously, making it one of the most complex joints in the human body. Its function relies on the coordinated performance of muscles, ligaments, and the jawbone.
Temperomandibular Disorders (TMD) encompass various conditions that cause problems in the muscles and ligaments handling jaw movements or within the joints themselves. Common indicators of TMD include:
- Pain in the jaw joint and surrounding muscles
- Limited movement or locking of the jaw
- Sounds like clicking or popping when the jaw moves
TMD symptoms can be misleading; ringing in the ears or headaches can be mistakenly attributed to other conditions.
When the coordination of the muscles surrounding TMJ is disrupted due to injury, arthritis, or habits like excessive gum chewing or nail-biting, TMD symptoms can manifest. Stress can exacerbate these issues, causing individuals to clench or grind their teeth unintentionally, particularly during sleep—known as bruxism—which further strains the TMJ.
While there is no singular confirmed cause for TMD, researchers suggest a combination of genetic tendencies, psychological stress, and physical health as potential contributors. Additionally, female hormones are being studied for possible links, as TMD prevalence is higher among women than men, particularly during the reproductive years.1
Understanding TMJ and TMD is crucial because mistreatment or ignorance about these conditions can lead to unnecessary surgeries or therapies that might worsen the problem rather than alleviate it. Recognizing the difference between normal joint sounds and symptoms indicating a disorder is essential for timely and appropriate treatment.

Common Symptoms of TMJ Disorders
TMJ disorders manifest through various symptoms that can significantly disrupt daily life. Among the most common are:
- Persistent jaw pain, which can radiate towards the neck or shoulder
- Uncomfortable clicking or popping noises during mouth movements
- Difficulties in opening or closing the mouth, ranging from mildly irritating to severely debilitating
The variability and intensity of TMJ symptoms can impact routine actions like chewing, yawning, or even conversational speech. The omnipresence of the jaw’s functionalities makes TMJ disorders a significant impediment to quality of life.
Symptoms such as earaches, headaches, and tinnitus (ringing in the ears) that often accompany TMJ issues can mislead sufferers and healthcare providers alike, mimicking the hallmarks of different medical problems.2 This multisymptomatic presentation underlines why personalized approaches are essential in the diagnosis and management of TMDs.
TMJ symptoms can vary in type and intensity from one person to another due to factors including individuals’ pain thresholds, the specific cause of their TMJ disorder, and lifestyle factors like stress levels and general health. Interestingly, the severity of the jaw misalignment doesn’t always correlate directly with the severity of pain or dysfunction—a slight misalignment might cause considerable pain for some, while others might endure noticeable anatomical alterations with little discomfort.
This variance emphasizes the necessity for individualized treatment plans that consider unique physiological conditions, individual lifestyles, and specific symptom patterns. By fostering a nuanced understanding of TMJ disorders, individuals can better handle their treatment options, leading to more sustainable and effective outcomes.
Factors Contributing to TMJ Disorders
Several factors are believed to contribute to the development of temporomandibular joint disorders (TMJ or TMD). Understanding these can help manage existing conditions better and possibly prevent the progression of TMJ disorders.
Genetic Predisposition: Genetics play a role in TMJ. Some individuals may inherit a natural susceptibility due to specific anatomical traits, such as variations in jaw shape or the composition of joint tissue, which can predispose one to joint dysfunction. This biological blueprint can manifest differently from one person to another, emphasizing the need for customized treatment approaches.
Injuries and Trauma: Physical impacts to the jaw or head regions, like those from sports injuries or accidents, can lead to TMD. Such traumas might shift the jaw out of its normal alignment, disrupt the smooth motion of the joint, or damage the cartilage disk, exacerbating stress on the joint.
Arthritis: Osteoarthritis and rheumatoid arthritis are common culprits that affect the TMJ, leading to degenerative changes in the joint. These forms of arthritis can deteriorate the cartilage that cushions the joint surfaces, altering joint function and leading to pain and restriction in movement.
Teeth Grinding and Clenching (Bruxism): This habit can exert excessive force on the joint structures and muscles. Many may not even be aware of this behavior since it often occurs during sleep. Bruxism not only stresses the joints but also the muscles, resulting in muscle fatigue and pain that can mimic or exacerbate TMD.
Poor Posture: Neck strain and abnormalities in spinal alignment influence jaw posture. Poor posture can encourage forward head position which in turn increases strain on the muscles and structures supporting the jaw. This habitual misalignment can alter the jaw’s mechanics and load distribution, leading to TMJ discomfort.
Hormonal Influences: Research indicates hormonal changes in women, particularly those related to estrogen, might correlate with higher incidences of TMD, suggesting a possible endocrinological element to TMJ disorders.3 This aspect requires further study but could explain why women are more prone to these disorders especially during certain phases of life such as pregnancy or menopause.
Lifestyle Factors: High-stress levels, diet, and overall lifestyle choices can also become significant contributors. A diet that requires strenuous chewing, or habits such as chewing gum excessively, can overwork the jaw muscles and joint. High-stress environments and lack of adequate rest disrupt bodily functions and healing, affecting muscular and joint health.
Understanding these factors provides insights into not just why TMJ disorders might appear but also offers pathways to manage symptoms proactively. Simple adjustments in everyday life—from ergonomic postures to stress management techniques—combined with professional medical advice, can make a substantial difference in managing TMJ disorders. This holistic approach emphasizes the importance of body-wide harmony and reinforces the need for attention to overall well-being as a strategy against such manifestations.
- Bagis B, Ayaz EA, Turgut S, Durkan R, Özcan M. Gender difference in prevalence of signs and symptoms of temporomandibular joint disorders: a retrospective study on 243 consecutive patients. Int J Med Sci. 2012;9(7):539-544.
- Tuz HH, Onder EM, Kisnisci RS. Prevalence of otologic complaints in patients with temporomandibular disorder. Am J Orthod Dentofacial Orthop. 2003;123(6):620-623.
- Warren MP, Fried JL. Temporomandibular disorders and hormones in women. Cells Tissues Organs. 2001;169(3):187-192.









